Scientists Discover New Fat Cell Types, Transforming Obesity Research
Findings reveal unique fat cell subpopulations, paving the way for personalized treatments for obesity
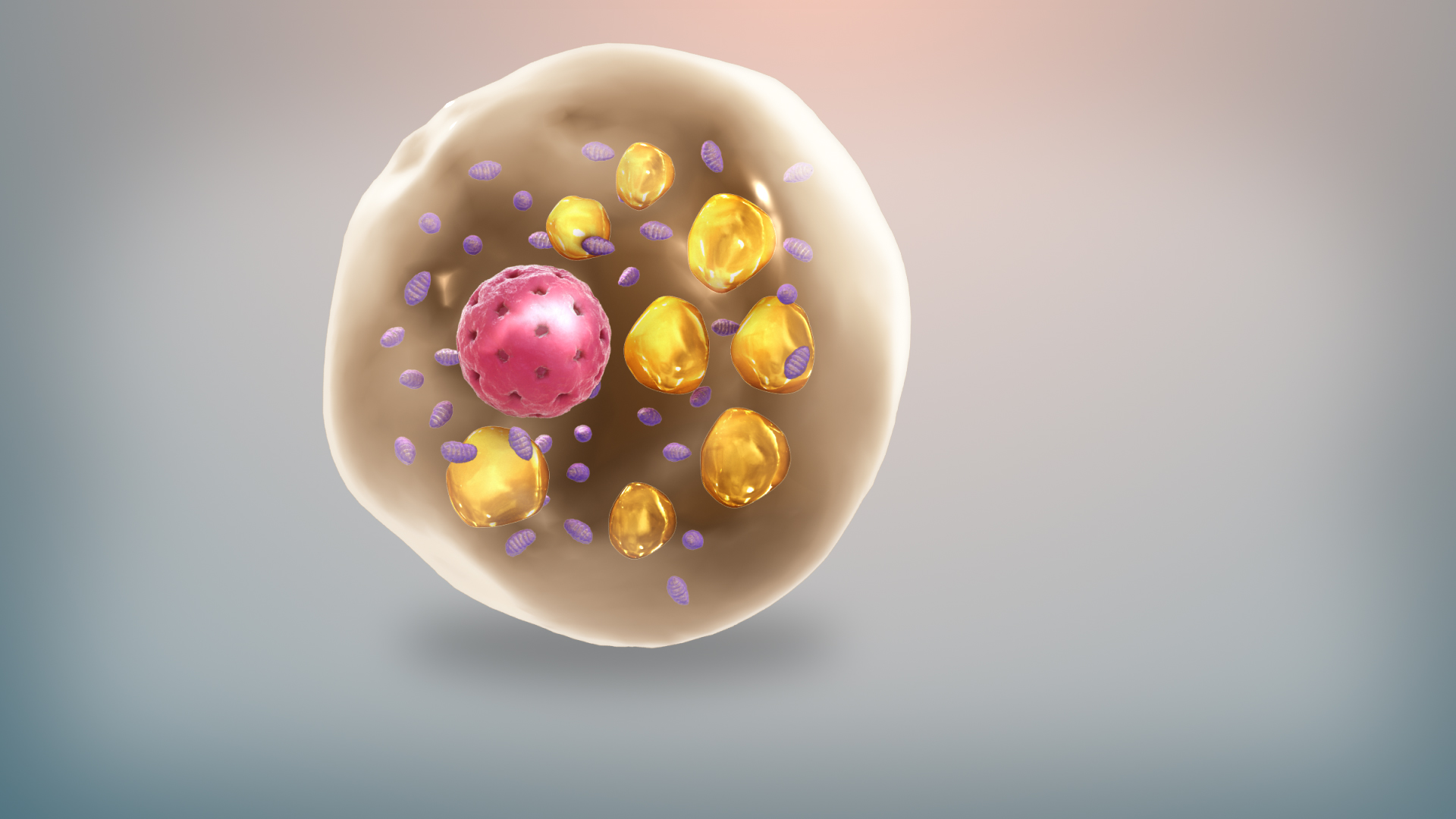
A groundbreaking international study has revealed a new level of complexity within human fat tissue, identifying distinct subpopulations of fat cells with specialized functions. Published in Nature Genetics, the Israeli-led research is the first to characterize the diversity of fat cells in subcutaneous and visceral fat tissues, shedding light on the cells’ role in health and disease.
Using innovative RNA-mapping technology, the researchers uncovered previously unidentified subtypes of fat cells and differences in intercellular communication within fat tissues. This discovery challenges the long-held view that fat cells, also known as adipocytes, merely store and release energy. Instead, the study confirms that fat tissue plays an active role in regulating key physiological processes through signals to the brain, blood vessels, liver, and pancreas. The findings could pave the way for more precise, personalized treatments for obesity and metabolic diseases.
The research was led by Esti Yeger-Lotem and Assaf Rudich from Ben-Gurion University of the Negev, in collaboration with Naomi Habib from the Hebrew University of Jerusalem, Matthias Blüher, Antje Körner, and Martin Gericke from Leipzig University, Germany, and Rinki Murphy from the University of Auckland, New Zealand.
Esti Yeger-Lotem, one of the lead researchers from Ben-Gurion University of the Negev, told The Media Line that most of the cells were “classical” fat cells. Research revealed a new subtype of fat cells with much higher mitochondrial content than others, suggesting that these cells might have a different function.
“This research gives us a new lens to look at fat tissue,” Yeger-Lotem said. “It’s not just about storing energy—these cells are playing a much bigger role in human health than we ever realized.”
Now, she said, the challenge is to understand the functions of the different fat cell types and how they relate to disease.
One of the fundamental questions the research aims to answer is why different fat tissues in the body behave differently. It has long been known that subcutaneous fat (beneath the skin) and visceral fat (around internal organs) function differently, with visceral fat being more inflammatory and more closely linked to metabolic diseases. Previous studies suggested that the cellular composition of these fat tissues was surprisingly similar.
“We knew that these two fat tissues were functionally and molecularly different,” researcher Assaf Rudich told The Media Line. “But previous studies looking at cell types in the tissues showed that they were too similar, which didn’t add up. We set out to find the more subtle differences that could explain this contradiction.”
The researchers found that the key difference was not in the kind of fat cells in each tissue but in how fat cells communicate within the tissue types.
“The differences were not where we initially expected them to be,” Rudich said. Rather than finding completely different types of fat cells in subcutaneous versus visceral fat, the researchers “found significant differences in how cells within each tissue interact and regulate gene expression.”
This discovery highlights that fat tissue function is determined not just by cell types, but also by complex signaling networks—which could be another key to understanding obesity-related diseases.
Another unexpected finding involved how fat cells develop over time. Originally, the researchers hypothesized that classical fat cells evolve into more specialized cells as part of their maturation process. But their analysis suggested the exact opposite.
Give the gift of hope
We practice what we preach:
accurate, fearless journalism. But we can't do it alone.
- On the ground in Gaza, Syria, Israel, Egypt, Pakistan, and more
- Our program trained more than 100 journalists
- Calling out fake news and reporting real facts
- On the ground in Gaza, Syria, Israel, Egypt, Pakistan, and more
- Our program trained more than 100 journalists
- Calling out fake news and reporting real facts
Join us.
Support The Media Line. Save democracy.
“What we actually found is that it’s the nonclassical adipocytes that appear first, and as they mature, they lose their unique functions and become classical adipocytes. This was completely opposite to what we expected,” Rudich said.
This finding suggests that the body’s ability to retain specialized fat cells may play a critical role in metabolic health, and that certain conditions—like obesity or insulin resistance—may affect how these cells transition from nonclassical to classical forms.
In order to perform their research, the team used human fat tissue samples from elective surgeries. But shortly after the researchers launched the study, the COVID-19 pandemic brought elective surgeries to a halt, cutting off their sample supply.
“During the pandemic, everything shut down,” Yeger-Lotem said. “For a long time, we were stuck without any data.”
It wasn’t until the pandemic was more controlled that the team was able to resume collecting and analyzing human fat tissue samples.
Even after regaining access to fat samples from elective surgeries, the study faced several major challenges, both technological and logistical.
One challenge involved the use of single-nucleus RNA sequencing technology. “It allows us to tag RNA molecules from individual cell nuclei with a unique barcode, which helps us map each fat cell at an unprecedented resolution,” Rudich said. “But implementing this technology was a huge technical challenge.”
Another, often overlooked, challenge was the complexity of multidisciplinary research.
Collaboration between different disciplines is crucial, but it’s also a challenge. It takes time and effort to align perspectives and methodologies. But when it works, it’s incredibly rewarding.
“A project like this requires expertise from multiple fields—computational biology, biomedical research, and clinical medicine,” Rudich said. “Collaboration between different disciplines is crucial, but it’s also a challenge. It takes time and effort to align perspectives and methodologies. But when it works, it’s incredibly rewarding.”
The study is part of the Human Cell Atlas Project, a global initiative that aims to map every cell type in the human body. Yeger-Lotem noted that that project was started by “two female scientists—one from England and one from MIT” who envisioned a global medical research project with publicly accessible findings.
It’s like mapping the world. We used to do that with geography, exploring new lands and identifying species. Now, we’re doing the same thing—but inside the human body. We are identifying new cell types that were never seen before, and that’s incredibly exciting.
“It’s like mapping the world,” Yeger-Lotem said. “We used to do that with geography, exploring new lands and identifying species. Now, we’re doing the same thing—but inside the human body. We are identifying new cell types that were never seen before, and that’s incredibly exciting.”
One of the most promising aspects of the study is the link it revealed between the newly identified fat cell subtypes and insulin resistance, a key factor in metabolic disorders.
“We found that these nonclassical adipocytes—which we didn’t even know existed before—are more prevalent in conditions of insulin resistance,” Rudich explained. “Now, the next step is to see if measuring their levels could actually predict how a patient will respond to a specific treatment.”
If further research confirms this link, the discovery could revolutionize precision medicine for obesity. Instead of using a one-size-fits-all approach, doctors could use a biomarker test to determine whether a patient is likely to develop obesity-related conditions and whether a medication like Ozempic or bariatric surgery will be more beneficial for the individual.
Getting from research to practical applications will take time. “This is what we consider basic research,” Rudich explained. “It’s not something that will immediately translate into a clinical treatment, but expanding human knowledge is the first step in the scientific process. Now that we’ve identified new fat cell types, we can start asking how they influence disease.”
Rudich emphasized that while people often want immediate applications, basic research is the foundation of scientific progress.
Everyone wants the fireworks—the big breakthrough that cures obesity overnight. But the reality is that progress happens in small, continuous steps. Expanding fundamental knowledge is the first step, and it’s crucial for developing future medical advances.
“Everyone wants the fireworks—the big breakthrough that cures obesity overnight,” he said. “But the reality is that progress happens in small, continuous steps. Expanding fundamental knowledge is the first step, and it’s crucial for developing future medical advances.”
While the study is still in its early stages, the researchers believe their findings will lay the groundwork for precision medicine in obesity treatment.
“This study has opened up many new questions,” Rudich said. “Now, we need to understand how these newly discovered fat cells function, how they influence disease, and how they can be used in medical treatments. We’re just at the beginning of this journey.”
With ongoing advancements in genomics, personalized medicine, and obesity research, the study’s findings could eventually play a key role in shaping the future of metabolic health.