Israel Can Lead Medical AI Revolution Internationally, Says MIT Professor
MIT professor Regina Barzilay argues Israel can set the global standard for testing and scaling clinical AI, from regulation and education to implementation inside large health providers
Israel’s combination of deep technological expertise and a relentless drive for innovation could position the country as a global leader in integrating artificial intelligence (AI) into healthcare, according to a leading international expert visiting Israel.
Prof. Regina Barzilay, a computer scientist at the Massachusetts Institute of Technology (MIT) and one of the world’s foremost figures in medical AI, said Israel is uniquely suited to play a central role in the AI in healthcare revolution. That role, she said, spans the full lifecycle of the technology, from evaluation and regulation to physician and patient education and real-world implementation.
Unlike many countries, Israel’s healthcare system brings providers and payers under the same organizational roof. That structure, Barzilay explained, creates an environment where innovation can move faster, data can be used more effectively, and AI tools can be tested and scaled with fewer barriers.
“Israel is really positioned to lead in this space country-wise,” Barzilay told The Media Line.
Speaking during her recent trip to Israel, which centered on the HealthTech AI Summit 2025, chaired by Prof. Ran Balicer, chief innovation officer at Clalit Health Services, Barzilay emphasized the critical role startups play in advancing artificial intelligence in healthcare. The summit took place at the end of December 2025.
Developing AI for healthcare, she said, depends heavily on innovation at the startup level.
“Israel has really very exciting developments,” Barzilay said. “Multiple companies are doing a great job in the AI and health space.”
At the same time, Barzilay acknowledged that adoption of what she described as fourth-generation AI tools still faces hesitation. One major obstacle is the lack of evidence that these technologies meaningfully change patient outcomes.
“Because the point is not only to detect [disease] earlier, but to show at the population level that it changes the outcomes,” she said.
Because the point is not only to detect [disease] earlier, but to show at the population level that it changes the outcomes
In breast cancer, for example, the goal is to prevent women from needing late-stage treatments, which are more expensive, more complex, and associated with poorer outcomes. Israeli companies, she added, are particularly well-positioned to demonstrate this kind of impact.
“If we’re talking about safe technology, you have much more agility,” Barzilay said. “You can bring this technology in and demonstrate at the population level. It really makes a difference. It will make it a much bigger sell and much more appealing for adoption in the United States and Europe.”
Barzilay was born in Ukraine and immigrated to Israel in her 20s. Today, she lives in the United States and is the School of Engineering Distinguished Professor of AI and Health in the Department of Computer Science, and the AI faculty lead at the MIT Jameel Clinic. She was recently named by Time magazine as one of the world’s most influential people in AI.
Her research focuses on developing machine learning methods for drug discovery and clinical AI. Earlier in her career, she worked extensively on natural language processing.
Balicer, who also serves as deputy director general at Clalit, invited Barzilay to participate in the summit and is collaborating with her on AI implementation in Israel. He told The Media Line that “Clalit is actively utilizing state-of-the-art scientific tools to provide our patients with predictive, proactive and individualized care, a major move from the existing reactive and uniform care that is the mainstream of modern healthcare.”
Give the gift of hope
We practice what we preach:
accurate, fearless journalism. But we can't do it alone.
- On the ground in Gaza, Syria, Israel, Egypt, Pakistan, and more
- Our program trained more than 100 journalists
- Calling out fake news and reporting real facts
- On the ground in Gaza, Syria, Israel, Egypt, Pakistan, and more
- Our program trained more than 100 journalists
- Calling out fake news and reporting real facts
Join us.
Support The Media Line. Save democracy.
According to Balicer, more than 100,000 individuals receive AI-driven care improvements each month at Clalit.
“We are proud to be working with Prof. Regina Barzilay on groundbreaking breast cancer screening studies of significant global importance that will hopefully allow us to turn these insights into care practice, as we already do in other validated domains,” he said.
Barzilay said doctors are no longer hesitant about adopting AI into their practices, as many were a decade ago. The main challenge today, she explained, is not convincing individual physicians, but driving system-wide change.
“The system needs to make this pathway a standard of care,” she said, explaining that AI tools should not be optional tests chosen on a case-by-case basis. Instead, they must be formally integrated into care guidelines and reimbursed by insurance.
“That’s why I am spending so much time in Israel, because I am working with Ran Balicer and Dr. Tanir Allweis, who is the head of the Breast Health Center at the Hadassah Medical Center in Jerusalem. We are all thinking together how to bring AI into our guidelines to really help the patients,” Barzilay said. “Somebody needs to put this effort and have the motivation to actually do this translation, because we don’t have many successful examples. It needs to be somebody who is, in a sense, a medical pioneer.”

Prof. Ran Balicer, deputy director general at Clalit, speaking at the HealthTech AI Summit 2025. (Courtesy: Rami Zarnegar)
Barzilay said she “randomly strolled” into the world of AI and healthcare. Trained as a computer scientist, she had not initially planned to work in medicine. That changed when, at age 43, she was diagnosed with breast cancer, the first case in her family.
As she went through treatment, Barzilay said she became acutely aware of the gap between how advanced AI had become in fields such as e-commerce and translation, and how little it had been applied in medicine. The experience took place in 2014, before what she describes as the major AI boom. She decided she wanted to help change that reality.
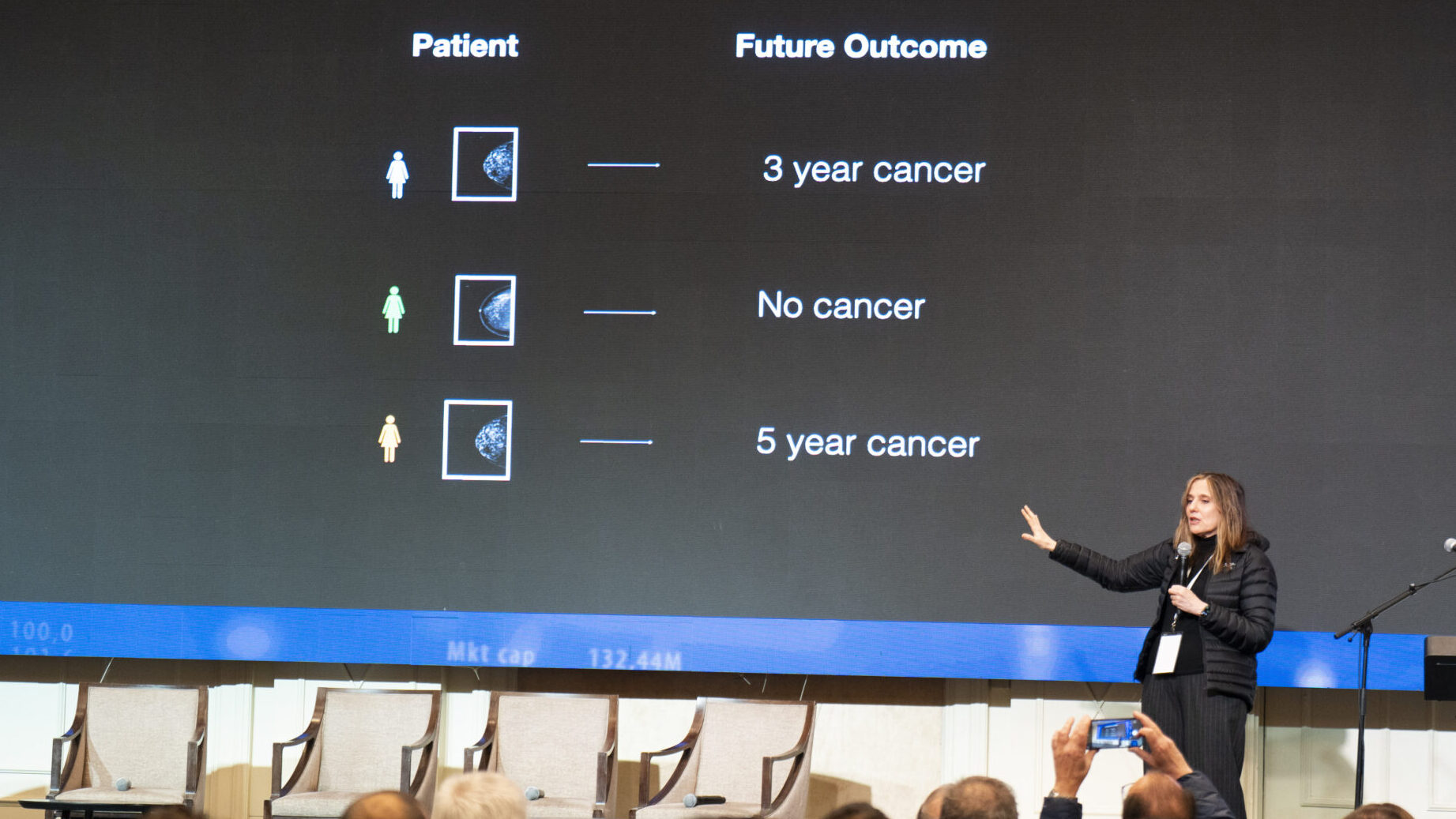
What captured her interest, Barzilay said, was the possibility of predicting which patients are likely to develop breast cancer based on their mammograms, something that does not exist today.
Currently, only a small group of patients carries known genetic mutations that can be tested to assess breast cancer risk. Barzilay set out to develop machine learning technologies capable of analyzing medical images and predicting the likelihood that a woman will develop breast cancer, expanding risk assessment far beyond genetic testing alone.
Doctors agree, she said, that breast cancer begins forming long before it becomes visible on imaging. There are subtle early signs, but they are extremely difficult for humans to detect. A machine, she explained, could potentially eliminate much of this uncertainty by collecting different pieces of information, “small clues,” and combining them into a single, coherent prediction.
“The existing question is, what is your future?” Barzilay said. “Today, we define the present, which is when the patient is diagnosed, based on the size of the tumor, when it is big enough that a human can really see it, or a radiologist can see it. Human vision is limited, even if you’re a radiologist. So, we are just diagnosing patients today. When it is invisible, it doesn’t mean that it’s not there. It is just that we cannot see it. By we, I mean the medical community.”
Barzilay turned this concept into action. Together with her team, she developed a machine learning tool called MIRAI, which identifies patterns associated with cancer development long before they are visible to the human eye. The tool was trained on data from nearly two million mammograms and is already showing significant promise.
“It actually works very robustly across many different populations,” Barzilay said.
She noted that her own breast cancer diagnosis was delayed by around two years. Through her research, she found that more than 70% of patients experience delayed diagnoses.
If you look today at a woman who is diagnosed with breast cancer, at least for one set of them, you could have seen it a year ago, and it was missed
“If you look today at a woman who is diagnosed with breast cancer, at least for one set of them, you could have seen it a year ago, and it was missed,” she said. “The machine can catch the cancer much earlier, or can at least identify that there is something wrong with this patient that requires a second look.”
Despite this potential, Barzilay said AI remains barely visible in everyday doctor visits. At the same time, medical error, at least in the United States, is the third leading cause of death.
“We’re not bringing AI to a perfect world. We’re bringing AI to the world of diagnosis and care, which is pretty broken,” Barzilay said. “There is more and more demand on the medical system, and it cannot provide enough resources. Doctors are tired, they make mistakes, or sometimes it’s just really hard to diagnose correctly. So, in this case, I think that the biggest question for the next five years is how to take all this, all of these great medical advances, and bring them into the system to make it more effective and cheaper.”
AI will not replace doctors, Barzilay emphasized, but it will require physicians to be trained differently. Computer science can help generate predictions, but doctors must interpret those predictions and decide what to do next. That, she said, is where AI ends and the physician’s role begins.
We’re not bringing AI to a perfect world. We’re bringing AI to the world of diagnosis and care, which is pretty broken
“They need to create a safe and secure pathway, deciding what to do with a patient who is high risk. It is not enough to tell a patient you are high risk,” she said. “In any other industry, we see so much AI, but in healthcare, doctors now have a responsibility to think about how to bring this technology, which is not perfect, but extremely powerful, to be safe and effective for the patient.”
Although Barzilay’s primary focus has been on breast cancer, she said the same technologies can be applied to diagnosing lung, prostate, and other forms of cancer. Beyond diagnostics, she added, artificial intelligence could also play a significant role in drug design.
Barzilay acknowledged ongoing concerns about bias and inequality associated with the use of AI. However, she argued that these issues already exist throughout the healthcare system.
There is a lot of bias and inequality in medicine, period
“There is a lot of bias and inequality in medicine, period,” she said, emphasizing that the presence of these risks should not deter the adoption of new technologies.
In fact, Barzilay said AI has the potential to reduce disparities rather than deepen them. Inequality in healthcare, she explained, often stems from differences in access to care. AI-driven tools could help level the playing field by standardizing diagnosis and decision-making across locations.
“If you have an automatic way of diagnosing, it doesn’t matter if you do it in Tel Aviv or Dimona, it will give you exactly the same outcome,” she said. “So, in this way, you can actually bring a higher quality of care to all.”